Coordinated Community Care Paramedicine In Santa Cruz County
Santa Cruz County Community Coordinated Care Model

Background
The Arizona Department of Health Services (ADHS) received the Centers for Disease Control and Prevention (CDC) State Public Health Actions to Prevent and Control Diabetes, Heart Disease, Obesity and Associated Risk Factors and Promote School Health Cooperative Agreement (1305 program). This 5 year project’s long term outcome is to “improve prevention and control of hypertension, diabetes, and overweight and obesity.” Chronic disease is a serious issue in Santa Cruz County. Cardiovascular disease is the leading cause of death, accounting for 25% of deaths, and diabetes is tied as the 4th leading cause at (4%).
Description of project
In 2015 a collaboration between The University of Arizona Prevention Research Center (AZPRC), Mariposa Community Health Center (MCHC), and the Rio Rico Medical and Fire District (RRFD), funded by ADHS 1305 program, resulted in the creation of a Coordinated Community Care Model (CCCM) and Implementation Plan. The purpose was to integrate and enhance emergency medical services (EMS) and community health center efforts to reduce the burden of chronic illness on individuals and health systems in Santa Cruz County, Arizona, and enhance multidisciplinary care teams for chronic disease management. The planning efforts resulted in development of training needs, communication protocols, evaluation, a logic model, and suggestions for coordinating complimentary systems of care. In 2016, ADHS invited the partners to convene to implement the plan.
In 2017, the partners worked to build on this foundation by expanding the model to include other EMS providers in Santa Cruz County; developing software systems to facilitate referrals and care coordination; and implementing ongoing evaluation and program improvements within each partner organization. This report describes goals and outcomes of the Santa Cruz County Community Coordinated Care Model (CCCM) during the August 1, 2016 - June 30, 2017 project year.
The project focuses on Domain 3, strategy 2 of the 1305 program:
- increasing team-based care, engaging non-physician team members such as Community Health Workers (CHWs or Promotoras de Salud) in hypertension and diabetes management,
- strengthening the Coordinated Community Care Program to decrease the burden of hypertension and diabetes on individuals and the health system in Santa Cruz County,
- reduce EMS utilization for non-emergency care,
- reduce health care cost,
- increase access to health services.
Description of Objectives and Activities
2.1. Through this funding ADHS shall collaborate with the contactor to continue and improve the system of care that includes the following:
|
Objectives |
Outcomes, Activities, and Notes |
|
2.1.1. Continue to enhance and expand the CIP/CHW program with a clearly defined scope of work and clinician oversight; within a community health clinic setting whose patient and potential-patient census includes a majority of patients from the following high-risk populations groups: African American women; Hispanic males; Asian/Pacific Islanders; and American Indians. |
The project Advisory Group consisting of representatives from partner organizations, and internal Work Groups within each partner organization identified key actions to enhance and expand the CIP/CHW programs: implement electronic referral and follow-up systems connecting EMS and MCHC, spread the referral system to other EMS providers, and conduct ongoing internal QI initiatives for related activities. |
|
2.1.2. Implementation of a coordinated response designed to increase direct efforts to link individuals without insurance or a medical home to medical services; |
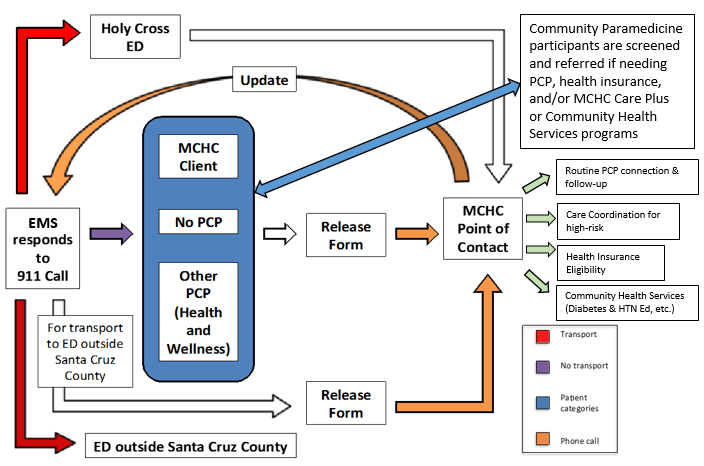
RRFD designed and implemented the methods to identify and refer patients without insurance or a medical home to MCHC. The electronic referrals are received by the MCHC Care Plus care coordination program, which contacts the patient to offer insurance eligibility and primary care medical home services. Reports are sent back to RRFD confirming the outcome of the outreach. |
|
2.1.3. Development of a new training plan which shall increase the capacity of Mariposa Community Health Center (MCHC) CHW’s and RRFD community paramedics to meet the needs of high intensity EMS users; |
RRFD implemented its training plan designed to train CIP and CHW staff from all partner organizations on the Community Coordinated Care Model (Communications, relevant services and structure of partner organizations), key topics in EMS/CIP and chronic disease management, and skills for coaching patients |
|
2.1.4. Development of an advisory group which shall monitor and evaluate implementation of the Coordinated Community Care Model (CCCM) and progress toward desired outcomes; |
The Advisory Group consisted of representatives from MCHC, RRFD, AzPRC, ADHS, and NFD met 3 times during the grant period |
|
2.1.5. Establish partnerships with at least 3 additional Fire Districts across Southern Arizona to increase awareness of Community Integrated Paramedicine Model; |
The partnership experienced delays in establishing new partnerships with fire districts. It took longer than anticipated to bring the new districts into the Community Paramedicine system, and the contracts to partner for this ADHS initiative piece weren’t executed until late in the project period. We are excited to establish new partnerships with Nogales Fire Department (NFD) and Tubac, and will continue efforts to include Sonoita-Elgin. |
|
2.1.6. Enrollment of identified patients into an educational program provided by CHW(s); |
MCHC CHWs enrolled 148 unique patients in Diabetes Education services. MCHC CHWs also provide weekly heart health classes at the Nogales Mexican Consulate that focus on hypertension called Su Corazón Su Vida (Your Heart Your Life) |
|
2.1.7. Referral of patients in other avenues of treatment/support as they are discovered through the intake process (such as diabetes education, tobacco cessation…etc.); |
Referrals for the CHW Diabetes Education and hypertension classes can come from any program in the clinic, community, or EMS system. Referrals from MCHC primary care providers and care coordination are sent via a task in the EHR system. Other Community Health Services programs refer patients through email or a warm hand-off, community paramedicine participants refer patients electronically through their care coordination software, and community outreach is conducted on an ongoing basis to inform and invite participants. |
|
2.1.8. Tracking of referral actions for follow up and to increase participation; |
The individual and program that sends the referrals receives notification of the outcome. MCHC CHWs record the outcomes of referrals in the MCHC EMR system, as well as responding electronically to Community Paramedicine programs through their EMR. |
|
2.1.9. Assessment of the patient’s self-efficacy to manage their chronic condition (HTN/DIAB); |
MCHC CHWs document in the patient’s EMR whether the patient has developed a self-management plan, including the details of it and the progress. With complex patients, they communicate directly with the PCP, either through the EMR, email, or in-person. |
|
2.1.10. Outreach to clinic’s geographical coverage area for hypertension and diabetes new-patient identification and medical home assignment (creating a community-clinic linkage); |
This outreach occurs through our partnership with the Community Paramedicine program, as well as attending community events and educating health and social service providers about the programs. |
|
2.1.11. Follow-up of the patient by the CHW to increase the successful self-management of hypertension/diabetes and decreased miss appointment rates; |
MCHC CHWs follow set protocols for patient outreach, including multiple phone attempts, problem-solving incorrect contact information, mailed letters, and working with the PCP or CIP partners to encourage participation. The CHWs asses each patient’s needs, conducting at least two visits, and more if the patients need further support |
|
2.1.12. Feedback to the primary care provider by the community health worker regarding the patient’s self-management of their blood pressure and diabetes; |
CHWs follow up and inform the PCP of the patient’s self-management plan and progress via EMR, email, and/or in-person contact. The MCHC Care Plus also documents their work and information in the EMR, including ED utilization, hospital admissions, and EMS utilization |
|
2.1.13. Reassessment of enrolled patients at the appropriate time to measure the HTN/DIAB self-efficacy and program/medication adherence; |
Once the patient completes CHW education services, the PCP continues to monitor their self-efficacy, adherence, and management, and can refer again for further services, including nutrition counseling with a RD, CDE, provided through Mariposa’s Vivir Mejor grant program. |
|
2.1.14. Implement a coordinated response design to increase direct efforts to link individuals without insurance or a medical home to medical services and decrease inappropriate of EMS; and |
During the project period, RRFD, Tubac and NFD Community Paramedics referred 70 unique patients to Mariposa Community Health Center’s Care Plus care coordination program, where they were triaged and assigned an appropriate level of follow-up. MCHC CHWs, care coordination, PCPs, and partner community paramedics all coordinate their work to educate patients about appropriate utilization of EMS vs. same-day appointments, on-call after hours answering service, and regularly scheduled appointments |
|
2.1.15. Implement a training plan which shall increase the capacity of Mariposa Community Health Center Community Health Workers (CHWs) and Rio Rico’s Fire Department Community Paramedics to meet the needs of high intensity EMS users. |
Training plan developed and implemented. See below for topics. |
Trainings
RRFD designed and carried out a training plan, focusing on providing Community Paramedicine (all fire districts) and MCHC staff with knowledge and skills for chronic disease management, patient care, safety, care coordination, and health system navigation. Topics included: Updated 2017 Community Coordinated Care Model (see below), Pharmacology for Emergency Responders (presented by MCHC Medical Director), Treat & Refer, patient privacy and legal considerations, Patient Education including “Teach-Back,” Fentanyl Safety for First Responders, Info Exchange & Collaboration for Paramedicine, and Navigating the Crisis System in Santa Cruz County. Staff from all partner organizations, as well as other organizations such as home health attended the trainings, so they also served as opportunities to develop deeper understandings of each other’s scope, organization, and services.
Updated 2017 Community Coordinated Care Model
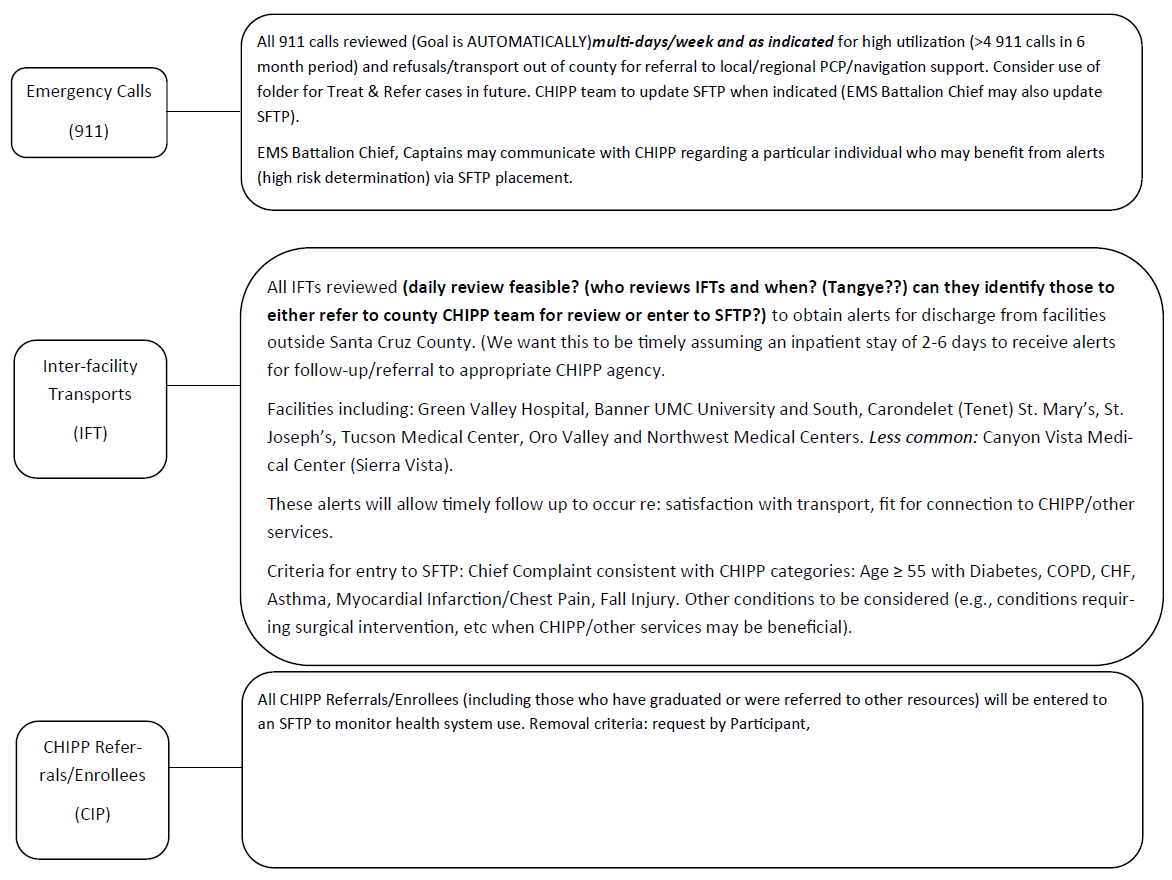
RRFD CHIP Referral Workflow
Program Evaluation
AzPRC has been engaged throughout the project to provide technical assistance and evaluation of the developing partnerships between MCHC and the EMS providers. For this project year, the team is focusing on a long-term goal of measuring the impact of CHW interventions by using a model to match each patient that has received CHW services with a similar patient who did not receive services and compare outcomes. The results of this will be available in winter 2017.
For internal evaluation, MCHC staff tracked the A1c and Blood Pressure of patients who received CHW Diabetes Education during the project period. Of 148 unique patients who received CHW services, MCHC staff were able to report on valid A1c and BP readings for 134 patients. Most patients received 2 CHW health education visits in the home or private meeting rooms on-site at MCHC. CHWs assessed patient need at the second visit and provided further follow-up as needed.
Baseline and target measures
- CHWs develop self-management plans with all the patients they provide services to, and document these plans in an electronic template in the EMR. Last project year, it was identified that this template was not a reportable field, so a self-management plan check box was identified elsewhere in the EMR that could be used to indicate a plan in a reportable way. In this year’s EMR report, just 8 of the patients had a documented self-management plan according to this check box. Program managers will assess the electronic documentation process to find out if this is a case of the data not being captured in the report or the workflow needing to be revised or better-implemented.
-
121 (90%) of the participating patients were diagnosed with diabetes
- Of those patients 106 had at least two HbA1c results on record. The number (%) of those patients with an A1c less than or equal to 9% increased from 69 (64%) to 72 (68%) between their last two or three readings.
-
118 of the participating patients have a hypertension diagnosis
- The number (%) of these patients who had “achieved blood pressure control” (according to program performance measures, a systolic BP/diastolic BP 140/90) increased from 94 (80%) to 103 (87%).
- 82 participating patients were diagnosed with both hypertension and diabetes
|
Su Corazón Su Vida Participant Characteristics |
||
|
Valid pre- and post-survey |
78 |
|
|
Average age |
53 (range 18-78) |
|
|
Female |
95% (74/78) |
|
|
MCHC Patient |
53% (41/78) |
|
|
Referred by doctor |
10% (8/78) |
|
|
Referred by friend/family |
21% (17/78) |
|
MCHC’s Vivir Mejor program provides heart health and hypertension education through Su Corazón Su Vida classes. The series of 5 classes are offered at the Mexican Consulate in Nogales on an ongoing, weekly basis. Results and discussion of program outcome have been taken from the Vivir Mejor Evaluation Report produced by the University of Arizona Prevention Research Center. During Vivir Mejor’s most recent program year, there were 300 visits to the SCSV classes, representing unique patients who attended at least 5 classes and filled out pre and post surveys. The pre-post surveys asked participants about the type of physical activity they practice, as well as the number of times they engage in that activity per day and week. The number of times participants engaged in physical activity per week increased from 3.2 times per week to 3.7 times per week. The percentage of participants who indicated that they do not do any physical activity decreased from 12% to 3%. The SCSV emphasizes the importance of incorporating physical activity into daily activities, and the percentage of participants who knew the CDC physical activity recommendations increased from 28% to 82%. All the participants learned the risks of sedentary behavior.
SCSV Participants were asked how satisfied they were with the Su Corazon Su Vida classes as part of the evaluation. 78% were very satisfied and 22% were satisfied with the classes. As a heart health curriculum, SCSV gives numerous concrete tips for participants to put into action to improve the health of both themselves and their family members. In general, participants embraced new practices such as not using table salt or adding salt to cooking water. The percentage of participants purchasing canned vegetables did not decrease, suggesting that the CHWs may want to try encouraging participants to rinse their canned vegetables before using or providing cooking demonstrations of frozen vegetables.
System Integration
The AzPRC participated in all partner meetings, as well as numerous planning phone conferences. Together, partners updated the CCCM Communications Plan, and developed electronic methods to share referrals in an efficient manner that complied with patient confidentiality. A total of 70 patients were referred from county Community Paramedicine programs (RRFD, NFD, and Tubac) to Mariposa Community Health Center’s Care Plus program. The program manager evaluated each case, triages them into categories: routine follow-up with an established MCHC patient, outreach to new MCHC patients who do not currently have a health care home, and high-risk patients who receive intensive Clinical Care Coordination services. Out of the 70 referrals, 18 (26%) were new to the MCHC system. The Care Plus manager reports back to the fire districts on a weekly basis with the outcomes of the referrals.
Success Stories
Green Valley Hospital contacted MCHC’s Community Health Services department regarding a patient who was about to be discharged. The patient had been admitted due to complications of uncontrolled diabetes. In addition, she had a communications impairment that meant she needed to communicate via text. Shortly after, MCHC received an electronic referral from the RRFD CHIP for the same patient. Due to the communication barriers and complexity of the case, MCHC CHW Diabetes Educator and RRFD Community Paramedic communicated frequently about the patient, including conducting a joint home visit. Through these efforts, the two programs assisted the patient to control her A1c, making her eligible for a surgery to address her impairment.
MCHC continues efforts to improve rates of referrals into appropriate CHW Diabetes Education and Care Coordination programs. During the project period the Community-Clinic Linkages Manager and CHW educators attended Adult Medicine Provider and Medical Assistant meetings to educate team members about available services, define the best population and criteria for referrals, explain the referral process, answer questions, and receive feedback for ways to improve. Staff also developed a more thorough matrix of all Community Health Services Department programs, with a special focus on better defining the available programs for adult chronic disease management. This resulted in increased referrals and improved provider and MA understanding of CHS services.
During a Diabetes Education home visit, a MCHC Diabetes Education CHW noticed a patient’s foot appeared red and swollen. The patient was in recovery from a recent surgery, so the CHW assisted the patient with obtaining a same day appointment with her surgeon in Tucson. The CHW also enrolled the patient in Mariposa Care Plus, which was able to assist the patient with navigation and connect to necessary specialist care.
This year marks a significant improvement in the management of shared patients and the functioning of the primary care/PCMH system – EMS System partnership. The scope of work between community paramedicine, care coordination, and CHW diabetes and hypertension programs is clearer and better operationalized, and all partners are more comfortably and efficiently able manage shared patients. This is due to stronger partnerships and improved data sharing software and workflows.
Challenges & Barriers
As with any new system, partners encountered glitches with electronic referrals. The Practice Fusion software is being used by Community Paramedicine as a care coordination and longitudinal patient record to complement their incident-based 911 system. It is a great resource for referrals to MCHC, however for unknown reasons, the MCHC CHW was locked out of her account. MCHC and RRFD staff tried multiple times to fix the issue, but have not been able to resolve it. They have created secure work-arounds in the meantime, but we hope in the future to develop a long-term solution.
Future Goals
In year 5 of the project, MCHC is working to continue increasing referrals for adult chronic disease education. We are exploring proactive, automated methods of identifying patients for CHW Diabetes Education and Care Coordination, including initiatives with the Quality Improvement team and purchasing software that can integrate data from multiple sources to predict poor health outcomes and facilitate care management. RRFD also continues to improve their software systems, working with the AZ Health Information Exchange to link in the state EMS database or at least create automated ways to transfer their EMS data into the HIE and receive alerts that they have been doing manually. The goal of both these efforts would be sharing information between MCHC and EMS providers in a way that is efficient and useful for everyone.